Mild Cognitive Impairment
Orchard at Brookhaven is a senior living community in Atlanta that supports people living with brain change. Our staff are undergoing a new method of training and use their knowledge and skill to support people in any stage of brain change. When people experience difficulty with memory or other functions of the brain, it’s possible they could be experiencing mild cognitive impairment (MCI) and not dementia.
What Is Mild Cognitive Impairment (MCI)?
Mild cognitive impairment (MCI) is the stage between the expected cognitive decline of normal aging and the more serious decline of dementia. It can involve problems with memory, language, thinking and judgment that are greater than normal age-related changes. But these changes aren’t severe enough to significantly interfere with daily life and usual activities.
Mild cognitive impairment may increase your risk of later developing dementia caused by Alzheimer’s disease or other neurological conditions. But some people with mild cognitive impairment never get worse, and a few eventually get better.
Types Of Mild Cognitive Impairment
There are two types of MCI. In both, symptoms are not severe, although they can be upsetting and disruptive.
Amnestic MCI
- Memory-specific and is marked by signs like forgetting conversations and misplacing items.
Non-amnestic MCI
- Involves changes in other brain activities regardless of whether you have memory loss.
- Problems with language (you lose your train of thought during a conversation)
- Attention (you have a hard time accomplishing tasks like bill paying)
- Spatial sense (you can’t find your way around a familiar place).
Signs & Symptoms Of Mild Cognitive Impairment
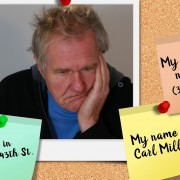
Symptoms of mild cognitive impairment include:
- Forget things more often.
- Forget important events such as appointments or social engagements.
- Lose train of thought or the thread of conversations, books or movies.
- Feel increasingly overwhelmed by making decisions, planning steps to accomplish a task or understanding instructions.
- Start to have trouble finding your way around familiar environments.
- Become more impulsive or show increasingly poor judgment.
If you have MCI, you may also experience:
- Depression
- Irritability and aggression
- Anxiety
- Apathy
Medical Condition & Lifestyle Impacts On MCI
Medical conditions and lifestyle factors have been linked to an increased risk of cognitive change. Some of these include:
- Diabetes
- Smoking
- High blood pressure
- Elevated cholesterol
- Obesity
- Depression
- Lack of physical exercise
- Low education level
- Infrequent participation in mentally or socially stimulating activities
- Stroke
- Traumatic brain injury
- Medication side effect
- Underlying health problem
- Sleep deprivation.
Diagnosing & Treatment For Mild Cognitive Impairment
There is no specific test to confirm a diagnosis of mild cognitive impairment (MCI). A doctor will decide whether MCI is the most likely cause of your symptoms based on the information you provide and results of various tests that can help clarify the diagnosis
Because MCI may be an early sign of Alzheimer’s disease, it’s important to see a doctor or specialist every 6 to 12 months.
There are no drugs or other treatments currently that are approved specifically for mild cognitive impairment. However, MCI is an active area of research. Clinical studies are underway better understand the disorder and find treatments that may improve symptoms or prevent or delay progression to dementia.
Orchard at Brookhaven is a senior living community in Atlanta that supports people living with brain change. Contact us for more information about our programs and how we can help you or your loved one.