Posts
Press Release~There is Such a Thing as Being Too Thin…
FOR IMMEDIATE RELEASE Contact: Irina Strembitsky & Orchard Senior Living
Phone: (404) 775-0488
Email: marketing@orchardseniorliving.com
Press Release
There is Such a Thing as Being Too Thin…
Improved nutrition outcomes are within reach for those living with dementia and other chronic illnesses.
Tucker, Georgia, April 2nd, 2018- After a year of research, testing and development, Orchard Senior Living is prepared to unveil our custom created Nutrition Therapy Program specifically designed for those with dementia, as well as other chronic illnesses that often lead to malnutrition or undernutrition. We developed this program because the current nutrition therapy options available have failed our residents as well as many others in the community.
A popular saying says, “We are what we eat.” A good diet is vital to everyone’s health, well-being, and quality of life. A person needs carbohydrates, protein, fat, fiber, minerals, vitamins, electrolytes, and water to survive. Obtaining the correct balance and quantities of these nutrients is essential. Insufficient nutrition and hydration can lead to deterioration of overall health, including mental health, as well as weight loss, dehydration, dizziness, increased risk of falls, prolonged recovery after surgery, change of mood, frequent colds, reduced strength, reduced mobility, reduced communication abilities, difficulty keeping warm, infections, as well as prolonged healing. Cognitive deficits such as Dementia, have a direct effect on a person’s nutrition. Malnutrition or undernutrition may occur at any stage of dementia. It is important to detect it and try to remedy this as early as possible.
Did you know? Up to 45 per cent of people living with dementia experience clinically significant weight loss over one year, and up to half of people with moderate or severe dementia have an inadequate food and nutritional intake. Some experience very quick weight loss, dropping to a withering 70-90 lbs. in a span of several months. As dementia advances, it’s difficult to ensure that those living with dementia are eating and drinking enough. These challenges increase the risk for malnutrition and can worsen other health conditions a person may already have. There are numerous reasons for poor appetite to develop, including depression, communication problems, sensory impairments, change in taste and smell, pain, tiredness, medication side effects, physical inactivity, and constipation. Some people with dementia may lose their ability to concentrate, so they become distracted while eating and stop eating as a result. Other people may have trouble using utensils or raising a glass. It may also be challenging to bring the food from the plate to their mouth. Some people may need to be reminded to open their mouth to put food in it or even to chew. Another common problem in more severe dementia cases is dysphagia, which is difficulty swallowing. Dysphagia can lead to weight loss, malnutrition, or dehydration. Over time you may find that your loved one’s appetite declines or the taste of food doesn’t appeal to them. Sensory changes in sight and smell can impact their ability to enjoy food and mealtimes. Their likes and dislikes for food and drink may be quite dramatic and different from the ones they held for many years. They may also find it difficult to tell you what they want to eat.
Dementia and Alzheimer’s Disease are not the only chronic conditions that can cause malnutrition or undernutrition. Other chronic conditions can often impact a person’s nutrition. Many illnesses cause what is called disease-related malnutrition. Many people living with Parkinson’s disease, suffer from muscle weakness or tremors, which can make eating very challenging. Other diseases that often cause nutrition deficiencies are cancer, liver disease, COPD, and CHF to name a few.
In many of these cases, the malnutrition and undernutrition are severe and all conventional methods have failed. Orchard’s state of the art Nutrition Therapy Program offers hope for this group, a group that has not responded to traditional nutrition methods. Orchard has partnered with Gordon Foods and their team of experts and dieticians, as well as with dementia specialists to bring this revolutionary nutrition therapy to the community.
Join us on April 12th from 4 pm-6 pm as we unveil our Nutrition Therapy Program to area professionals who are interested in helping our community battle this difficult problem. Event attendees will be able to taste a variety of nutrition therapy options such as Cake a Boo, Sherberita, and Strawberry Smash. This event will be held at Orchard at Tucker, 2060 Idlewood Rd, Tucker GA 30084. For questions or to RSVP for the event please email marketing@orchardseniorliving.com.
Tips for Seniors (and their Families) on Downsizing Their Home
Sometimes seniors leave a big house to move to a senior community or assisted living. This new home may be more secure, healthier, and happier, but it’s also likely to be smaller.During this process, a family has two main tasks to focus on: helping their senior loved ones settle comfortably with valued possessions and preparing a house for sale. Downsizing with respect and practicality is important to both goals. Here are some transition to assisted living tips that you may find helpful during the process:
Cherished Possessions
It can be hard to separate possessions that truly matter from things that need to be let go. Be patient with anyone who lived in the house and feels attached to it, and expect difficult feelings as natural to the process. Just don’t let objects take priority over anyone’s well-being: the bottom line is that not everything can stay. If there’s not enough time to sort through everything with sensitivity, temporary storage may be the answer. Families can rent a unit or offer some home storage space so that no one feels stressed by any rush.
If there is time to sort through belongings, have seniors choose what goes to the new residence, what they would like distributed to family or friends, and what can be donated to charity. If children or grandchildren are just starting out in a new home themselves, seniors may be glad to contribute necessities they no longer need. Donations can also be satisfying when an item will help a stranger in need. Some charities will pick up goods and furniture by appointment.
It’s true that homes sometimes collect material things over decades, if homeowners don’t purge periodically. No family member should face exhaustion, or neglect their own family or livelihood, over each and every thing in a crowded house. Make sure the downsizing plan is appropriate for everyone. If the house is going on the market, sellers must declutter it of most contents and deep-clean. It must be staged to attract buyers. Seniors and their families need to commit to being understanding with each other, and also to getting the house sold efficiently.
There are tools that use local sales data to help you find the best time to sell in Atlanta. Statistics for 2014-2016 show that June and July are the best months for closing if you want the highest price possible on the home sale. Thus, listing in April or May, and having the house ready to show then, reaps sales about 7% over the yearly average. If your priority is to sell your house quickly, the data says you should aim for the same two months, since homes closing in June or July spend 1-2 weeks less on the market than those closing in other months of the year.
If you’re debating when to sell your house, find and ask an experienced local agent about the current state of the market and how you can maximize your home sale.
Written by Lin Nulman.
There is Such a Thing as Being Too Thin…
Improved Nutrition outcomes are within reach for those living with Dementia and other chronic illnesses.
A popular saying says, “We are what we eat.” A good diet is vital to everyone’s health, well-being, and quality of life. A person needs carbohydrates, protein, fat, fiber, minerals, vitamins, electrolytes, and water to survive. Obtaining the correct balance and quantities of these nutrients is essential. Insufficient nutrition and hydration can lead to deterioration of overall health, including mental health, as well as weight loss, dehydration, dizziness, increased risk of falls, prolonged recovery after surgery, change of mood, frequent colds, reduced strength, reduced mobility, reduced communication abilities, difficulty keeping warm, infections, as well as prolonged healing. Cognitive deficits such as Dementia, have a direct effect on a person’s nutrition. Malnutrition or under nutrition may occur at any stage of dementia. It is important to detect it and try to remedy this as early as possible.
Did you know? Up to 45 per cent of people living with dementia experience clinically significant weight loss over one year, and up to half of people with moderate or severe dementia have an inadequate food and nutritional intake. Some experience very quick weight loss, dropping to a withering 70-90 lbs. in a span of several months. As dementia advances, it’s difficult to ensure that those living with dementia are eating and drinking enough. Eating difficulties are also very common in those living with Alzheimer’s Disease. These challenges increase the risk for malnutrition and can worsen other health conditions a person may already have. There are numerous reasons for poor appetite to develop, including depression, communication problems, sensory impairments, change in taste and smell, pain, tiredness, medication side effects, physical inactivity, and constipation. Some people with dementia may lose their ability to concentrate, so they become distracted while eating and stop eating as a result. Other people may have trouble using utensils or raising a glass. It may also be challenging to bring the food from the plate to their mouth. Some people may need to be reminded to open their mouths to put food in it or even to chew. Another common problem in more severe dementia cases is dysphagia, which is difficulty swallowing. Dysphagia can lead to weight loss, malnutrition, or dehydration. Over time you may find that your loved one’s appetite declines or the taste of food doesn’t appeal to them. Sensory changes in sight and smell can impact their ability to enjoy food and mealtimes. Their likes and dislikes for food and drink may be quite dramatic and different from the ones they held for many years. They may also find it difficult to tell you what they want to eat.
Dementia and Alzheimer’s Disease are not the chronic conditions that often cause malnutrition or under nutrition. Other chronic conditions often impact a person’s nutrition. Many illnesses cause what is called disease-related malnutrition. Many people living with Parkinson’s disease, suffer from muscle weakness or tremors, which can make eating very challenging. Other diseases that often cause nutrition deficiencies are cancer, liver disease, COPD, and CHF to name a few.
In many of these cases, the malnutrition and under nutrition are severe, and all conventional methods have failed. Orchard’s State of the Art Nutrition Therapy Program offers hope for this group, a group that has not responded to traditional nutrition methods. Orchard has partnered with Gordon Foods and their team of experts and dieticians, as well as with dementia specialists to bring this revolutionary nutrition therapy to the community.
Join us on February 27th 4 pm-6 pm as we unveil our Nutrition Therapy Program to area professionals who are interested in helping our community battle this difficult problem. This event will be held at; Orchard at Tucker, 2060 Idlewood Rd, Tucker GA 30084. For questions or to RSVP for the event please email marketing@orchardseniorliving.com.
Dementia, I Will Give You My Memory, If You Leave Me My Personality
What Does Dementia Mean to the Average Person?
Dementia is a general decline in cognitive ability severe enough to interfere with daily life. Memory loss is one example. Dementia is not a specific disease. Dementia is a term that describes a wide range of symptoms associated with a decline in memory and other thinking skills severe enough to reduce a person’s ability to perform everyday activities. People with dementia often have problems with short-term memory recall, keeping track of a wallet or other possessions, paying bills, planning and preparing meals, remembering appointments or traveling out of the neighborhood. Dementia is progressive, as symptoms start out slowly and gradually get worse. As Dementia progresses, individuals notice increased memory loss, mental decline, confusion especially in the evening hours, disorientation, inability to speak or understand language, making things up, mental confusion, or inability to recognize common things.
What Does Dementia Mean to Those of Us Who See it Every Day?
Although the above examples of dementia symptoms are true, and do indeed interfere with a person’s everyday life, they are not a full picture of dementia symptoms. When dementia steals memory, language, thinking and reasoning, these new deficits are referred to as “cognitive deficits” of the disease. The term “behavioral and psychiatric symptoms” describes a large group of additional, and in my opinion most devastating, symptoms that occur to at least some degree in many individuals with dementia. In early stages of dementia, many experience personality changes such as irritability, apathy, anxiety or depression. In later stages, many experience sleep disturbances, mixing up their days and nights, agitation such as physical or verbal outbursts, combativeness, combativeness while getting care, refusal to get care, general emotional distress, restlessness, continuous pacing, shredding paper or tissues, yelling for no apparent reasons, delusions, paranoia, misperceptions, or hallucinations.
Real Life Example of a Behavioral Change.
Linda is 87 in the moderate stage of dementia. She retired as a Vice President of a company. Her family told me that she was known for her business acumen and immaculate appearance. Her outfits were always perfectly put together, her makeup and hair flawless. Today, due to the dementia, it is a struggle to get Linda to take a shower, comb her hair, or get any grooming what so ever. She refuses to wear makeup and will very rarely agree to get her hair done. She refuses manicures and pedicures that she used to get weekly for over 40 years. It is extremely painful for her family to watch Linda, who was always so well put together, now refuse to get her hair done, and be combative when any grooming is attempted. Unfortunately, this type of a personality change is common to those with dementia. Dementia has stripped Linda of her desire to look nice and be well groomed. In a year’s time, dementia has changed grooming habits Linda had for over 40 years.
Real Life Example #2
Lynn is 84 in the moderate stage of dementia. She worked as party planner before she retired. She was always very social and the life of the party. Lynn remained social into the mild stages of dementia. During the tail end of the mild stage, Lynn was still social, however when she would be around others they would ask her questions about her family and herself that she had trouble answering due to her dementia. Each time Lynn was not able to answer a question, she would leave the social or the event immediately. Shortly after, Lynn refused to participate in any of the hobbies and socials she enjoyed her whole life. This is another common example of dementia changing a person’s personality, and converting a social butterfly into a reclusive butterfly.
Lynn was reclusive and isolated for several months. Finally, her family decided to move her to the Orchard at Tucker, a community that specializes in cognitive care and engagement for those with cognitive deficits. Lynn’s family provided the Orchard with a detailed profile as well as her history and the Orchard engagement team came up with a detailed plan to combat Lynn’s new reclusive personality. The engagement team took all the information they were given, and they were able to create an Enabling Environment for Lynn. To learn more about enabling an environment see http://stage-osl.daveminotti.com/creating-an-enabling-environment-is-key-to-providing-dementia-care/)
With the creation of a new enabling environment, Lynn slowly started to participate in some activities. Although the Orchard engagement team did several things to modify her environment, one such modification was surrounding Lynn with other residents that were on her cognitive level. They also made sure that all team members were aware of Lynn’s history and her strong desire to mask her dementia. When everyone was aware of Lynn’s dementia, and the other resident around her also had dementia, no one asked Lynn any difficult questions, and her dementia never stood out to others. This one environmental change alone led to Lynn participating in activities daily, although never to the extent she used to participate prior to the dementia. Environmental modifications are very helpful, but they can never make up for all the damage caused by dementia. In Lynn’s case, her personality change could have been minimized if an enabling environment was created sooner. I believe Lynn’s personality change was so significant, so quickly, at least in part due to Lynn losing her self-esteem by not being able to answer the questions asked, and her struggle to hide her dementia from those that were noticing. This is a prime example of a personality change that dementia caused, that could have been lessened by an earlier intervention.
The Take Away..
I have spoken with so many loved ones of those with dementia, and they have all agreed, that the behavioral changes caused by Dementia that are hardest on their loved one, as well as the entire family. Losing your memory is nothing compared to becoming a different person. Also, it is the behavioral changes caused by dementia that impact one’s life, much more negatively than memory loss. It is much easier to compensate for a person’s memory loss than to compensate for extreme anxiety, paranoia, combativeness, or refusal to get care. These behavior symptoms are rarely talked about. When you ask the average person what dementia means, they will say dementia causes memory loss. Most people do not realize how many other terribly negative symptoms are caused by dementia. They don’t realize that if dementia just caused memory loss, most people with dementia would have a much better quality of life. Most people don’t understand the devastation dementia causes. Dementia causes comprehensive memory loss, not just memory loss of what happened yesterday, or what time it is, but in many cases the loss of one’s personality. Very rarely are the personality changes positive. Almost always these behavioral personality changes negatively impact a person’s quality of life. These changes often create a completely different person, often unrecognizable to friends and family. As dementia progresses, these changes happen quickly and become more and more noticeable. It is important to understand that they are still the same person inside. They have not changed on the inside, the way they now communicate with the outside world has changed. Dementia causes a person to have a battle, both internal and external, a battle for who they were, and how they were ones perceived.
Creating an Enabling Environment is Key to Providing Dementia Care
How does Dementia effect a person’s ability to enjoy their hobbies and participate in activities?
Nutrition Therapy at Each Level of Dementia Care
 What is a common challenge for those with Dementia?
What is a common challenge for those with Dementia?
Challenges at mealtime are extremely common for those with dementia. These mealtime challenges will change as dementia progresses. There are distinct and separate challenges that are associated with early, middle and late stage dementia.
What are the common mealtime challenges for those in the Early Stage of Dementia?
- Forgetfulness
- Loss of concentration
- Changes in food preferences
- Reporting that foods taste bland (foods previously enjoyed)
- No longer enjoying favorite restaurants
- Unable to hold attention through a meal
- Distracted by the environment at mealtime
What are the common mealtime challenges for those in the Moderate Stage of Dementia?
- Confusion and unawareness of surroundings, place and time
- Appetite increase and weight gain
- Decreased appetite and weight loss
- Failure to understand proper use of utensils
- Refusal to sit during meal times- pacing, wandering
- Increased difficulty with word finding and decision making
- Unable to recognize food temperatures
- Unable to see food as food (may think food is poisoned)
- Unable to recognize food items once liked
- Hiding of food
What are the common mealtime challenges for those in the Severe Stage of Dementia?
- Preference for liquids over solids, due to appetite change or lack of swallowing ability
- Aggressive or combative behaviors during a meal

- Clenches jaw, or closed fist when attempting to feed or be fed
- Refusal to eat due to unknown reasons (variety reasons could be at play)
- Inability to self feed, not being used to being fed
- Swallowing impairments ranging from mild to severe
- Weight loss despite regular caloric intake (can also be due to increase activity due to increased anxiety)
What are some important tips for a creating a dining environment for those with Dementia?
- Tableware contrast ( avoid white plates on white linens)
- Too many utensils
- Avoid high gloss floors
- Natural light is best
- Avoid a distracting dining environment with too many items on the table
- Make sure the table and chair is sturdy, and of the right height
- Simplified dining room is best
- All food served at once is usually best (although there are some exceptions)
- Offer finger foods (avoid finger food that are too intricate or rare)
What if the above tips do not work?
If the above tips do not help with the challenges presented at mealtime, your team needs to take further steps to make sure that nutritional needs are met and your resident with Dementia is getting adequate caloric intake and the necessary nutrition.
The first thing your team needs to do is to do a full assessment of each person’s unique situation and determine the specific deficiencies caused by the mealtime challenges. During the assessment your team must set goals and prioritize the deficiencies, identify resources needed based on the severity of a person’s challenges. Your team needs to also identify possible behavioral and nutrition interventions such as a change of dining environment. Finally your team should specify the time and frequency of the intervention.
What’s Next?
Please check back soon for Part II of this article
Comprehensive Dementia Care Includes Educating Family Caregivers
What is Dementia?
Dementia is the loss of many or all cognitive abilities, such as thinking, remembering, and reasoning, as well as behavioral abilities to such an extent that it interferes with a person’s daily life and activities. Dementia ranges in severity from the mildest stage, when it is just beginning to affect a person’s functioning, to the most severe stage, when the person must depend completely on others for basic activities of living.
What happens to many caregivers of loved one’s with Dementia?
Caring for a loved one with dementia can be challenging and, at times, overwhelming. Frustration is a normal and valid emotional response to many of the difficulties of being a caregiver. While some irritation may be part of everyday life as a caregiver, many caregivers feel feelings of extreme frustration. Frustration and stress negatively impact their physical health and may cause a caregiver to be physically or verbally aggressive towards their loved one.
What are the Warning Signs of caregiver frustration?
-
Shortness of breath or knot in the throat
-
Stomach cramps or chest pains
-
Headache which could be severe
-
Compulsive eating or excessive alcohol consumption
-
Increased smoking or drug use
-
Lack of patience or the desire to strike out
- Sleepless Nights
Why is dementia education important for families caring for loved ones with dementia?
Dementia is called a family disease, because the chronic stress of watching a loved one slowly decline affects everyone. Education helps caregivers understand their loved one’s challenging behaviors and how to respond to them correctly. Often starting out caregivers use intuition to help decide how to respond to a challenging behavior. Unfortunately, dealing with Dementia is counter intuitive, and often the right thing to do is exactly opposite of what seems like the right thing to do. Caregiver education also helps families understand the progression of their loved ones disease. They will learn what to expect and therefore have an opportunity to prepare for these changes. Changes in their loved one’s cognitive abilities wont be a shock every time they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
How can communities help educate dementia care givers?
- community workshops and educational forums
-
lecture series followed by discussion
-
support groups
-
skill-building groups, case studies
-
individual counseling and training
-
family counseling
-
technology-based training that can be done at home
The Takeaway…
At Orchard Senior Living, we find all of the above methods useful. Each of these methods should be utilized by a community whose priorities are to provide comprehensive dementia care to their residents and their family caregivers. Currently we offer our 3 Step Navigating the Transition Program to individual and families. We also offer our monthly 2 hour Live and Learn Series which combines skill building, lecture, discussion, as well as an educational forum. Both of these programs are presented by a dementia specialist, specializing in family counseling and dementia training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.
training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.
The Biggest Misconception about the Dementia Brain in Dementia Care
Why is our brain so important?
The brain is the most important organ in the human body. It controls and coordinates actions and reactions, allows us to think and feel, and enables us to have memories and feelings. Furthermore the brain runs everything. It is the guiding, maintenance, and managing system for hundreds of a human beings needed abilities.
When does dementia occur? The quick answer…
Dementia occurs when the brain is damaged by disease. Sometimes it is one part of the brain, sometimes it is multiple parts.
To understand dementia, we must first understand the brain…
The brain can be divided into different parts: the brain stem and cerebellum, the limbic system, and the cerebral hemispheres. Each part has different functions.
Brain stem and cerebellum…
The brain stem is at the base of the brain. It controls basic bodily functions such as heartbeat and breathing. The cerebellum
controls balance and posture. Breathing and staying upright are things that we normally do automatically.
The limbic system…
The limbic system is deep inside the brain. It links the brain stem and the cerebral hemispheres. The limbic system includes structures with key roles in memory (the hippocampus) and emotions (the amygdala). The limbic system is the first part of the brain to develop and is sometim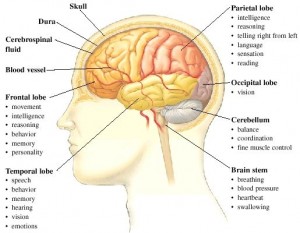 es referred to as our “primal brain” and manages many of our survival reflexes. It includes the amygdala which is in charge of the “flight, fright, fight response.
es referred to as our “primal brain” and manages many of our survival reflexes. It includes the amygdala which is in charge of the “flight, fright, fight response.
Cerebral hemispheres…
The tissue that makes up three-quarters of the brain is called the cerebrum. It is responsible for consciousness, memory, reasoning, language and social skills. A deep groove that runs from the front to the back of the cerebrum divides it into left and right halves: the two cerebral hemispheres.
The left and right cerebral hemispheres have different functions. For example, language is usually dealt with mainly by the left hemisphere. In contrast, awareness of where things are around us is usually dealt with mainly by the right hemisphere.
The lobes….
The four lobes are: occipital, temporal, parietal and frontal lobes. Each lobe does different things, though they also work closely together.The lobes are responsible for our senses. There are 5 ways human beings take in information (data) about the world through their nervous system.. What you see, hear, touch/feel, smell, and taste.
you see, hear, touch/feel, smell, and taste.
The lobes are some of the first areas effected by Dementia..
Dementia diseases often impact abilities in the occipital lobe of the brain which affect a person’s visual field. Dementia commonly affect the temporal lobes asymmetrically; typically attacking left temporal lobes before the right. This means more loss in language stored on the left, and more preserved skills for much longer. In dementia, different forms of damage to the lobes in the brain can cause someone to become either over-emotional or lacking in feelings. This is one of the reasons that a person with dementia exhibits changes in behavior along with memory loss. Sometimes the changes in behavior may be more pronounced than the memory loss. In these cases, many times dementia gets misdiagnosed since common thinking is, that dementia causes just memory loss.
What is the biggest misconception about the dementia brain and those with dementia?
Emotional memory is stored in the hippocampal area and is commonly a preserved skill. Persons living with dementia may not remember the details of what happened, but will almost always remember how an experience made them feel. Traditional thinking is if someone does not remember what they did specifically shortly after they did it, their day has less relevance, their life should be less purposeful. This is the biggest misconception in traditional dementia care. Those with dementia may get to a point that they don’t remember going to a great concert the next day, or helping to bake and delivering cookies to a police department, but they remember till almost the very end how much they enjoyed the concert, and how good they felt delivering those cookies over to those officers.
The Take Away…..
Orchard Senior Living is determined to bring a new type of dementia care to those inflicted with dementia. It is an engagement focused cognitive care model, where we focus on activities that will be stored in our residents’ emotional memories which they will have with them till they take their last breath.