Comprehensive Dementia Care Includes Educating Family Caregivers
What is Dementia?
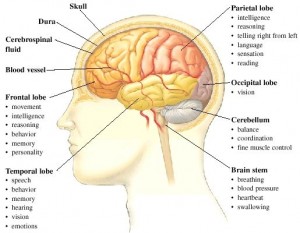
Dementia is the loss of many or all cognitive abilities, such as thinking, remembering, and reasoning, as well as behavioral abilities to such an extent that it interferes with a person’s daily life and activities. Dementia ranges in severity from the mildest stage, when it is just beginning to affect a person’s functioning, to the most severe stage, when the person must depend completely on others for basic activities of living.
What happens to many caregivers of loved one’s with Dementia?
Caring for a loved one with dementia can be challenging and, at times, overwhelming. Frustration is a normal and valid emotional response to many of the difficulties of being a caregiver. While some irritation may be part of everyday life as a caregiver, many caregivers feel feelings of extreme frustration. Frustration and stress negatively impact their physical health and may cause a caregiver to be physically or verbally aggressive towards their loved one.
What are the Warning Signs of caregiver frustration?
-
Shortness of breath or knot in the throat
-
Stomach cramps or chest pains
-
Headache which could be severe
-
Compulsive eating or excessive alcohol consumption
-
Increased smoking or drug use
-
Lack of patience or the desire to strike out
- Sleepless Nights
Why is dementia education important for families caring for loved ones with dementia?
Dementia is called a family disease, because the chronic stress of watching a loved one slowly decline affects everyone. Education helps caregivers understand their loved one’s challenging behaviors and how to respond to them correctly. Often starting out caregivers use intuition to help decide how to respond to a challenging behavior. Unfortunately, dealing with Dementia is counter intuitive, and often the right thing to do is exactly opposite of what seems like the right thing to do. Caregiver education also helps families understand the progression of their loved ones disease. They will learn what to expect and therefore have an opportunity to prepare for these changes. Changes in their loved one’s cognitive abilities wont be a shock every time they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
How can communities help educate dementia care givers?
- community workshops and educational forums
-
lecture series followed by discussion
-
support groups
-
skill-building groups, case studies
-
individual counseling and training
-
family counseling
-
technology-based training that can be done at home
The Takeaway…
At Orchard Senior Living, we find all of the above methods useful. Each of these methods should be utilized by a community whose priorities are to provide comprehensive dementia care to their residents and their family caregivers. Currently we offer our 3 Step Navigating the Transition Program to individual and families. We also offer our monthly 2 hour Live and Learn Series which combines skill building, lecture, discussion, as well as an educational forum. Both of these programs are presented by a dementia specialist, specializing in family counseling and dementia training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.
training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.