Posts
Creating an Enabling Environment is Key to Providing Dementia Care
How does Dementia effect a person’s ability to enjoy their hobbies and participate in activities?
Nutrition Therapy at Each Level of Dementia Care
 What is a common challenge for those with Dementia?
What is a common challenge for those with Dementia?
Challenges at mealtime are extremely common for those with dementia. These mealtime challenges will change as dementia progresses. There are distinct and separate challenges that are associated with early, middle and late stage dementia.
What are the common mealtime challenges for those in the Early Stage of Dementia?
- Forgetfulness
- Loss of concentration
- Changes in food preferences
- Reporting that foods taste bland (foods previously enjoyed)
- No longer enjoying favorite restaurants
- Unable to hold attention through a meal
- Distracted by the environment at mealtime
What are the common mealtime challenges for those in the Moderate Stage of Dementia?
- Confusion and unawareness of surroundings, place and time
- Appetite increase and weight gain
- Decreased appetite and weight loss
- Failure to understand proper use of utensils
- Refusal to sit during meal times- pacing, wandering
- Increased difficulty with word finding and decision making
- Unable to recognize food temperatures
- Unable to see food as food (may think food is poisoned)
- Unable to recognize food items once liked
- Hiding of food
What are the common mealtime challenges for those in the Severe Stage of Dementia?
- Preference for liquids over solids, due to appetite change or lack of swallowing ability
- Aggressive or combative behaviors during a meal

- Clenches jaw, or closed fist when attempting to feed or be fed
- Refusal to eat due to unknown reasons (variety reasons could be at play)
- Inability to self feed, not being used to being fed
- Swallowing impairments ranging from mild to severe
- Weight loss despite regular caloric intake (can also be due to increase activity due to increased anxiety)
What are some important tips for a creating a dining environment for those with Dementia?
- Tableware contrast ( avoid white plates on white linens)
- Too many utensils
- Avoid high gloss floors
- Natural light is best
- Avoid a distracting dining environment with too many items on the table
- Make sure the table and chair is sturdy, and of the right height
- Simplified dining room is best
- All food served at once is usually best (although there are some exceptions)
- Offer finger foods (avoid finger food that are too intricate or rare)
What if the above tips do not work?
If the above tips do not help with the challenges presented at mealtime, your team needs to take further steps to make sure that nutritional needs are met and your resident with Dementia is getting adequate caloric intake and the necessary nutrition.
The first thing your team needs to do is to do a full assessment of each person’s unique situation and determine the specific deficiencies caused by the mealtime challenges. During the assessment your team must set goals and prioritize the deficiencies, identify resources needed based on the severity of a person’s challenges. Your team needs to also identify possible behavioral and nutrition interventions such as a change of dining environment. Finally your team should specify the time and frequency of the intervention.
What’s Next?
Please check back soon for Part II of this article
Comprehensive Dementia Care Includes Educating Family Caregivers
What is Dementia?
Dementia is the loss of many or all cognitive abilities, such as thinking, remembering, and reasoning, as well as behavioral abilities to such an extent that it interferes with a person’s daily life and activities. Dementia ranges in severity from the mildest stage, when it is just beginning to affect a person’s functioning, to the most severe stage, when the person must depend completely on others for basic activities of living.
What happens to many caregivers of loved one’s with Dementia?
Caring for a loved one with dementia can be challenging and, at times, overwhelming. Frustration is a normal and valid emotional response to many of the difficulties of being a caregiver. While some irritation may be part of everyday life as a caregiver, many caregivers feel feelings of extreme frustration. Frustration and stress negatively impact their physical health and may cause a caregiver to be physically or verbally aggressive towards their loved one.
What are the Warning Signs of caregiver frustration?
-
Shortness of breath or knot in the throat
-
Stomach cramps or chest pains
-
Headache which could be severe
-
Compulsive eating or excessive alcohol consumption
-
Increased smoking or drug use
-
Lack of patience or the desire to strike out
- Sleepless Nights
Why is dementia education important for families caring for loved ones with dementia?
Dementia is called a family disease, because the chronic stress of watching a loved one slowly decline affects everyone. Education helps caregivers understand their loved one’s challenging behaviors and how to respond to them correctly. Often starting out caregivers use intuition to help decide how to respond to a challenging behavior. Unfortunately, dealing with Dementia is counter intuitive, and often the right thing to do is exactly opposite of what seems like the right thing to do. Caregiver education also helps families understand the progression of their loved ones disease. They will learn what to expect and therefore have an opportunity to prepare for these changes. Changes in their loved one’s cognitive abilities wont be a shock every time they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
they happen, because a caregiver will be prepared for them to happen. Caregivers will also learn which skills are typically retained the longest and can tailor their interactions with their loved ones’ based on these abilities.
How can communities help educate dementia care givers?
- community workshops and educational forums
-
lecture series followed by discussion
-
support groups
-
skill-building groups, case studies
-
individual counseling and training
-
family counseling
-
technology-based training that can be done at home
The Takeaway…
At Orchard Senior Living, we find all of the above methods useful. Each of these methods should be utilized by a community whose priorities are to provide comprehensive dementia care to their residents and their family caregivers. Currently we offer our 3 Step Navigating the Transition Program to individual and families. We also offer our monthly 2 hour Live and Learn Series which combines skill building, lecture, discussion, as well as an educational forum. Both of these programs are presented by a dementia specialist, specializing in family counseling and dementia training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.
training. We also offer a support group facilitated by a Clinical Social Worker. We are currently in the final stages of bringing a web based training program to our residents’ family members to help them on a daily basis. We believe comprehensive dementia care is more than the traditional model of a secure memory care, care partners helping with ADLs, and an Activity Calendar. Comprehensive Dementia Care is taking care of a resident and their families from the time prior to a move in, as well as throughout their entire journey. To find out about the Comprehensive Care Programming at the Orchard call us at 404-775-0488 for a private counseling appointment to determine how we can help. If we can’t help you in your unique situation, will will provide you with the information for those who can.
Delicious Puree Recipes for Assisted Living & Memory Care
One of my favorite puree recipes are Mango Moose Cups. They are easy to make, and most importantly very delicious.
- 1 tsp gelatin powder
- 2 tbsp water
- 5 oz mango puree
- 2 tbsp granulated white sugar (or more to taste)
- 5 oz heavy whipping cream
Dissolve gelatin into 1 tbsp of water. Heat remaining 1 tbsp water until it is hot/almost boiling and add to gelatin, stirring until gelatin is fully dissolved. Add gelatin and puree into blender and mix on high speed until fully blended. In a stand mixer, add 2 tbsp sugar and heavy cream and whip on high speed until stiff peaks form. Slowly add puree into the whipped cream, folding it into the cream until completely mixed and uniform in color. Pour into individual portion cups and refrigerate to set.
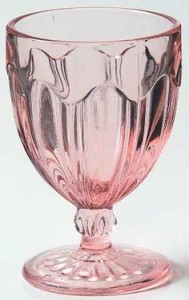
It is very important to use pretty glassware that is the right size for the right person. One person may require a 4 oz glass and one a 12 oz glass. It is important to note that personal preferences are very important in all food preparation. Here is an example of a pretty glass.
 If we follow this wonderful, easy to make recipes you will get:
If we follow this wonderful, easy to make recipes you will get:
(please note that the garnishment on top of the mouse is for decoration designed to make the cup look appetizing. Decoration should be removed prior to consumption for those that are on a pure diet)


